Blood Clot from Pulled Tooth: 10 Things to Know After Extraction
Having a tooth removed is a significant dental procedure. Once the anaesthetic wears off and you leave the dentist’s chair, the most critical part of your recovery begins: the formation and protection of the blood clot from the pulled tooth. This tiny, gelatinous structure is your body’s natural plaster, and protecting it is the single most important factor in ensuring a smooth recovery without complications.
After the teeth extraction, you might be wondering, “Is my healing normal?” or “Can I still enjoy my favourite hawker food?” This comprehensive guide covers everything you need to know about the blood clot after tooth extraction, tailored specifically for patients navigating the recovery process.
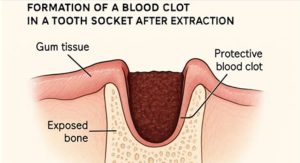
1. How Blood Clot Forms After Tooth Extraction
The formation of a blood clot is the very first step in your body’s healing mechanism. Immediately after your dentist or oral surgeon removes the tooth, the denture socket (the hole in the bone where the tooth used to be) fills with blood. This is not a sign of a problem; it is a physiological necessity. Within minutes, natural proteins in your blood, such as fibrin, begin to clump together to form a mesh-like structure. This creates a plug—the blood clot from the pulled tooth—that seals the wound.
This clot serves two vital functions. Firstly, it acts as a protective shield over the exposed jawbone and the sensitive nerve endings buried deep within the denture socket. Secondly, it serves as a foundation for the growth of new soft tissue and, eventually, new bone. Without this clot, healing halts, and you are left vulnerable to infection and intense pain.
For a molar extraction blood clot, the plug is generally larger because molar roots are deeper and wider than incisors. Consequently, the clot takes slightly longer to stabilise. It is crucial to understand that this clot is fragile in the first 24 to 48 hours. The stability of this clot determines how quickly you can return to your daily routine.
2. Dry Socket vs. Blood Clot
After your dentist pulls the tooth, a blood clot from the pulled tooth forms in the socket. It looks like a dark scab and protects the area while it heals. If you notice that a blood clot fell out after extraction, leave it alone and don’t try to touch or remove it.
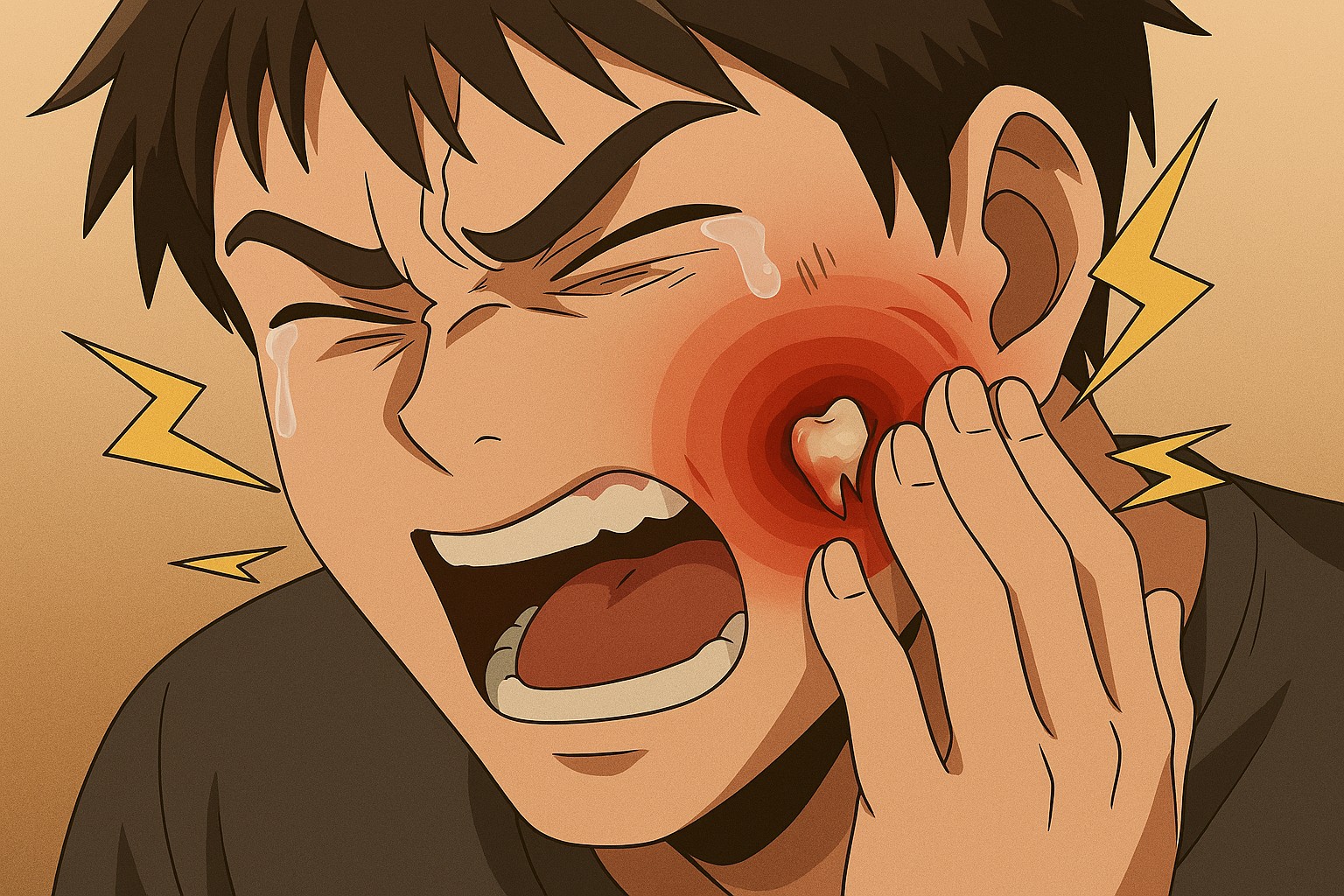
But one of the most common fears patients have is developing alveolar osteitis, commonly known as “dry socket.” This condition occurs when the blood clot falls out after extraction or dissolves before the wound has healed. In countries like Singapore, where humidity is high, bacteria proliferation can occur if oral hygiene isn’t maintained, but dry socket is primarily caused by mechanical dislodgement.
Understanding the difference between a healthy recovery and a dry socket is essential for knowing when to visit a General Practitioner (GP) or return to your dental clinic. A healthy clot usually appears as a dark red or brownish scab within the gum hole. In contrast, dry socket exposes the whitish bone underneath and is accompanied by a distinct, throbbing pain that radiates to the ear or neck.
Comparison: Healthy Healing vs. Dry Socket
The following table outlines the key differences to help you identify the state of your extraction site.
| Feature | Healthy Blood Clot | Dry Socket (Alveolar Osteitis) |
|---|---|---|
| Visual Appearance | Dark red, brown, or sometimes white/yellow granulation tissue (new skin). | Empty-looking hole; visible white bone; looks “dry”. |
| Pain Level | Dull throb that decreases daily; manageable with Panadol or Nurofen. | Sharp, intense radiating pain that worsens after Day 3; medication often ineffective. |
| Taste/Smell | Slight metallic taste initially, fading quickly. | Persistent foul taste and bad breath (halitosis). |
| Timing | Forms immediately; stabilises in 24-48 hours. | Usually occurs on Day 3 to Day 5 after extraction. |
| Source: National Dental Centre Singapore (NDCS) & Mayo Clinic Guidelines. | ||
3. Managing Pain While Preserving Blood Clot
Pain management is a delicate balance. You want to eliminate discomfort, but you must avoid actions that could dislodge the clot. Dentists will typically prescribe analgesics like Paracetamol (Panadol) or Ibuprofen (Nurofen). For more complex surgeries, such as wisdom tooth removal, they might prescribe stronger painkillers like Tramadol or Arcoxia.
It is vital to take these medications exactly as prescribed. Do not wait for the pain to become excruciating before taking a dose. However, be cautious with aspirin, as it acts as a blood thinner and can prevent the blood clot from pulled tooth from stabilising, causing prolonged bleeding.
If you are experiencing discomfort, avoid placing heat packs on your face in the first 48 hours. In the tropical climate, you might feel hot already, but applying heat externally can increase blood flow to the area, leading to more swelling and potential bleeding. Stick to a cool environment—stay in an air-conditioned room if possible—to keep your body temperature regulated.
4. Swelling and How to Reduce It
Swelling is a natural inflammatory response, especially after a surgical extraction involving bone removal. You might look in the mirror and feel like a chipmunk, but this is temporary. The swelling typically peaks around Day 2 or Day 3.
To manage this, use an ice pack wrapped in a thin towel. Apply it to the outside of your cheek adjacent to the extraction site. The standard protocol is 20 minutes on, followed by 20 minutes off. You can purchase gel ice packs from local pharmacies like Watsons, Guardian, or Unity. In a pinch, a bag of frozen peas works brilliantly as it moulds to the shape of your jaw.
Keep your head elevated, even when sleeping. Propping yourself up with an extra pillow helps reduce hydrostatic pressure in the head, which minimises both throbbing pain and swelling. If you are resting on a sofa, ensure you don’t lay completely flat.
5. How to Control Post-Extraction Bleeding and Protect the Blood Clot
Some oozing of blood is normal for the first 24 hours. Your saliva might look pink, which can be alarming, but it is usually a mix of a little blood and a lot of saliva. However, active bleeding needs management to ensure the pulled tooth blood clot remains intact.
Steps to Control Bleeding:
- Firm Pressure: Bite down firmly but gently on the sterile gauze pad provided by your dentist. Maintain this pressure for at least 30 to 45 minutes. The pressure helps the fibrin mesh to form.
- Tea Bags: If bleeding persists after changing the gauze twice, try using a moistened black tea bag (like Lipton or Dilmah, commonly found in Singaporean kitchens). Tea contains tannic acid, which helps contract blood vessels and assists in clotting. Bite on the tea bag for 30 minutes.
- Rest: Avoid strenuous activities. No gym sessions, jogging at East Coast Park, or heavy lifting for at least 3 days. Elevated blood pressure can burst the newly formed clot.
To answer how to protect the pulled tooth blood clot after tooth extraction, you must avoid creating negative pressure in your mouth. This means:
- No sucking: Absolutely no straws. When you buy a drink from a Kopitiam or a Bubble Tea shop, remove the lid and drink from the rim.
- No spitting: Do not spit forcefully into the sink. If you need to clear your mouth, let the fluid drool out naturally or use a tissue to wipe.
- No smoking: Smoking creates suction and introduces chemicals that delay healing. This is strictly prohibited for at least 72 hours.
Read more: 11 Best Home Remedies to Cure Bleeding Gums 2025
6. Cleaning Your Mouth Safely After Tooth Extraction
Oral hygiene is non-negotiable, even with a wound in your mouth. A dirty mouth can lead to infection, which destroys the pulled tooth blood clot. However, the technique must be modified.
For the first 24 hours, do not rinse your mouth at all. Let the clot stabilise. After 24 hours, you can begin gentle saltwater rinses. Dissolve half a teaspoon of salt in a cup of warm water. Gently move your head side to side to swish the water around—do not puff out your cheeks or use vigorous gargling motions. Let the water fall out of your mouth into the sink.
You should continue to brush your other teeth but avoid the extraction site completely for the first few days. You can use a soft-bristled toothbrush (often labelled as ‘sensitive’ in local supermarkets like NTUC FairPrice or Cold Storage) to clean the surrounding areas carefully.
Read more: Should You Brush Your Teeth Before or After Breakfast?
7. Foods to Eat After Tooth Extraction
Diet plays a massive role in recovery. In Singapore, we are blessed with a variety of soft food options, but we must also be wary of our spicy and hot favourites. The goal is to eat nutrient-rich foods that require minimal chewing.
Singaporean Post-Extraction Diet Guide
| Category | Recommended (Safe) | Avoid (Danger Zone) |
|---|---|---|
| Main Meals | Congee/Porridge: Ensure it is lukewarm, not piping hot. Fish or minced pork porridge is excellent.
Steamed Egg: Soft and easy to swallow. Mee Sua: Cooked until very soft (soup style). |
Laksa/Curry: Too spicy and irritates the wound.
Rice: Small grains can get lodged in the socket. Sticky Rice (Bak Chang): Too sticky, can pull the clot. |
| Snacks & Desserts | Tau Huay (Soya Beancurd): Eat it cold or room temperature.
Yoghurt/Pudding: Smooth texture is perfect. Ice Cream: Cup only (no cone), avoid flavours with nuts or chocolate chips. |
Keropok/Chips: Sharp edges can cut the gum.
Popiah: The skin requires tearing action which is bad for the jaw. Durian: Heaty and fibrous; best avoided initially. |
| Beverages | Ice Water/Isotonic Drinks: (100Plus – non-carbonated version or let it go flat).
Soya Bean Milk: nutritious and cooling. |
Hot Kopi/Teh: Heat dissolves clots.
Alcohol: Interferes with medication and healing. Bubble Tea with Pearls: The pearls require chewing and the straw is a major risk. |
| Dietary recommendations adapted for local Singaporean context. | ||
8. Follow-Up Care and Checkups
Most simple extractions do not require a follow-up unless complications arise. However, if you had stitches (sutures), you might need to return to your dental clinic in 7 to 10 days to have them removed. Some clinics use dissolvable stitches, which disappear on their own within two weeks.
If you experience severe pain that is not controlled by painkillers, excessive bleeding after 24 hours, or a fever, you should contact your dentist immediately. In an after-hours emergency, major hospitals like Singapore General Hospital (SGH) or the National Dental Centre (NDC) have emergency services. Keep your dental appointment card handy, and remember that dental procedures are often claimable under specific Medisave schemes if surgery was involved, so keep your receipts.
9. Healing Timeline for Blood Clot and Extraction Site
Healing is not an overnight process. Understanding the timeline helps manage expectations regarding the blood clot from pulled tooth.
- First 24 Hours: Critical period. The blood clot forms. Bleeding stops. Focus on rest.
- Days 2-3: Swelling peaks and then begins to subside. The clot is stabilising. Granulation tissue begins to form.
- Days 7-10: The hole begins to close as gum tissue grows over the clot. Stitches may be removed. You can slowly reintroduce solid foods, chewing on the opposite side.
- Weeks 2-4: The socket is mostly healed with soft tissue. However, the bone underneath takes months to fully remodel.
Note that a molar extraction blood clot may follow a slightly slower timeline due to the size of the wound. Be patient with your body.
10. Tips for Preventing Future Complications
Once you have navigated the immediate danger zone, the long-term goal is to prevent infection and ensure the bone heals correctly. Continue to rinse with saltwater after meals for at least two weeks. This prevents food debris from getting stuck in the healing socket, which can smell bad and cause infection.
If you were given a syringe by your dentist (common for wisdom tooth surgeries), start using it only when instructed (usually after day 5 or 7) to gently flush out food from the socket. Do not use it too early, or you risk blasting the clot out.
Summary & Key Takeaways
Protecting the blood clot from pulled tooth is the cornerstone of a complication-free recovery. From the moment you leave the clinic, your priority is to maintain the clot’s stability by avoiding suction (straws, smoking), eating appropriate soft foods like porridge and Tau Huay, and maintaining gentle oral hygiene. Remember, pain is normal, but excruciating pain that appears days later is a sign of dry socket and requires professional attention.
By following these Singapore-tailored guidelines, you can ensure your recovery is as swift and comfortable as possible. If you are ever in doubt, call your dental clinic—local dentists prefer you ask questions rather than suffer in silence.
Deep Dive: Common Questions About Tooth Extraction Clots
1. Can a blood clot from a pulled tooth fall out?
Yes, the blood clot can be dislodged, a condition known as dry socket. This usually happens due to negative pressure in the mouth caused by sucking on straws, smoking, spitting vigorously, or sneezing with the mouth closed. Mechanical disturbance, such as poking the site with a tongue or toothbrush, can also cause the clot to fall out physically.
2. Can blood clot from the pulled tooth be prevented?
You cannot prevent the formation of a blood clot; in fact, you want it to form! However, you can prevent the loss of the blood clot (dry socket). To do this, strictly follow post-operative instructions: avoid straws, smoking, and hot foods for the first few days. Keep the mouth clean with gentle saltwater rinses after 24 hours to prevent infection from dissolving the clot.
3. What to do if a blood clot comes out of a tooth extraction?
If you suspect the blood clot fell out after extraction, contact your dentist immediately. Do not try to force a new clot to form by poking it. Your dentist may place a medicated dressing (often containing clove oil/eugenol) into the socket to soothe the bone and relieve pain. Continue taking painkillers as prescribed until you can see the dentist.
4. What does a normal tooth extraction blood clot look like?
A normal blood clot appears as a dark red or brownish scab sitting inside the tooth socket. Over the first few days, it may develop a whitish or yellowish film on top—this is often fibrin and new tissue (granulation tissue), not pus. As long as there is no severe pain or foul smell, this appearance is part of the normal healing process.
5. Can a blood clot reform after being dislodged?
The original primary blood clot will not reform once it is lost. However, the body will eventually heal the wound through secondary intention, meaning tissue will grow from the sides of the socket to cover the exposed bone. This process is much slower and more painful than primary healing. Your dentist can induce a new bleed to encourage a new clot in severe cases, but typically, they treat the pain while the body heals naturally over a longer period.
6. How long does it take for a molar extraction blood clot to heal?
A molar extraction blood clot takes longer to fully resolve than smaller teeth. The gum tissue typically closes over the socket within 2 to 3 weeks. However, the underlying bone remodelling takes 3 to 6 months. You should feel significantly better and be able to eat normally (with caution) after about 7 to 10 days.
References
- Penn Pacific Dental Center. Oral Surgery and Wisdom Tooth Removal in Singapore
- Mayo Clinic. (2024). Dry socket. A comprehensive medical overview explaining causes, symptoms, risk factors, and prevention of dry socket after tooth extraction.
- Cleveland Clinic. (2024). Dry Socket: Symptoms, Causes & Treatment.