Many people look for practical ways on how to know if your wisdom tooth is infected. Recognising the early signs of wisdom tooth infections allows you to manage symptoms safely, even before you receive professional assessment. This guide walks you through the key symptoms, what causes these infections, and what you can safely do at home until you receive proper dental care.
What Are Wisdom Tooth Infections
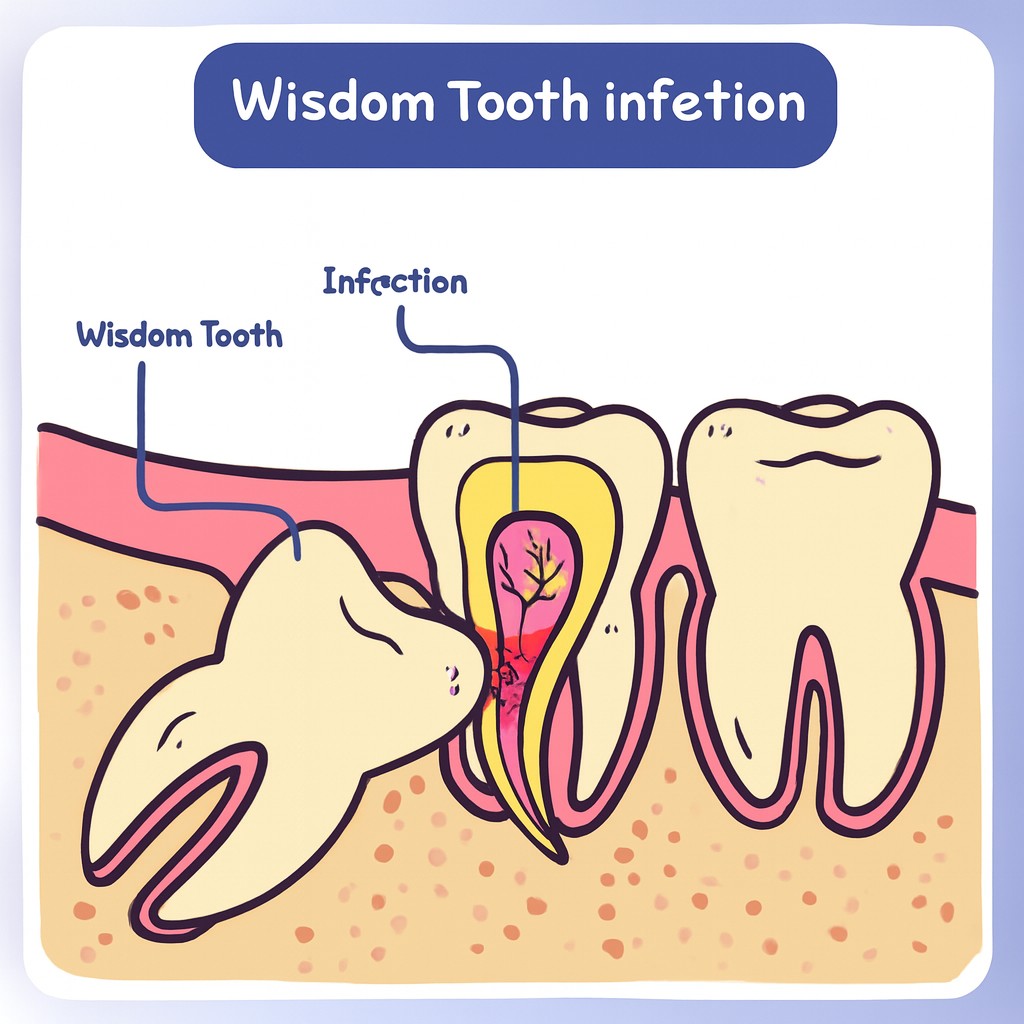
Wisdom tooth infections are one of the more common oral health issues, especially in the late teens and early twenties. These infections occur when the third molars, commonly called wisdom teeth, do not fully emerge or become impacted. An impacted tooth is one that grows at an angle or fails to break through the gum line properly, creating small pockets where food particles, plaque, and bacteria can accumulate. This accumulation leads to tooth inflammation and pain.
During long waiting times at polyclinics, recognising the early signs of infection becomes crucial. Delayed treatment can allow bacteria to spread, affecting not only adjacent teeth and gums but sometimes even leading to more serious complications such as jaw abscesses or cellulitis, which can affect facial tissue.
How to know if your wisdom tooth Is Infected: Symptoms
Pain and Tenderness in the Jaw
Persistent pain is often the earliest and most noticeable sign of an infected wisdom tooth. The discomfort may start as a mild ache, but it can escalate over days, particularly when chewing or opening your mouth widely. Many patients report a throbbing sensation that radiates towards the ear or temple. Tenderness can also be felt when gently pressing on the jaw or near the back of the mouth, indicating that your immune system is reacting to bacterial invasion.
Swelling and Redness in the Gum Area
Swelling and redness around the gums adjacent to the wisdom tooth are classic indicators of infection. In some cases, the gum may become shiny or overly firm, and minor bleeding can occur during brushing. Infections can extend swelling to the cheeks or jaw, sometimes resulting in noticeable facial asymmetry, which may make speaking and eating uncomfortable.
Bad Breath or Unpleasant Taste
A wisdom tooth infection can release odorous compounds, causing persistent bad breath (halitosis) or a sour, metallic taste in the mouth. This symptom often persists despite thorough brushing and flossing, signalling that the underlying issue is bacterial rather than simply plaque buildup.
Difficulty Opening the Mouth or Chewing
Inflammation around the wisdom tooth can impact the muscles and ligaments of the jaw, causing stiffness and limited mobility. This can make everyday activities like eating, speaking, or yawning uncomfortable. Some individuals notice a “lockjaw” sensation or increased discomfort when attempting to chew on the affected side.
Fever and General Malaise
Systemic symptoms such as mild fever, fatigue, and general malaise can indicate that the infection is affecting more than just the local area around the tooth. While often not life-threatening at first, these symptoms show that your immune system is actively fighting bacterial infection, and they should not be ignored, particularly during prolonged polyclinic wait times.
Pus Discharge
Visible pus around the wisdom tooth or in the gum pocket is a definitive sign of infection. Pus is composed of dead white blood cells, bacteria, and tissue debris, representing the body’s immune response. The presence of pus indicates a more severe infection that requires professional evaluation and often antibiotics or dental procedures.
How Tooth Inflammation Develops Around Wisdom Teeth
Understanding how to know if your wisdom tooth is infected becomes easier once you recognise how tooth inflammation typically starts and spreads around partially erupted molars. Inflammation around wisdom teeth typically begins when bacteria infiltrate the gum tissue surrounding a partially erupted or impacted tooth. Food debris, plaque accumulation, and limited accessibility for brushing create ideal conditions for bacterial growth. Once bacteria invade, the immune system responds by sending white blood cells to the area, causing redness, swelling, and discomfort. Left unmanaged, this inflammatory response can progress to form an abscess, which may lead to more severe complications, including fever, lymph node swelling, and systemic infection.
The process often starts subtly, with minor discomfort that worsens over days or weeks. In Australia, dentists often see patients presenting with early inflammation due to delayed access to care, particularly in public polyclinics where waiting times can extend to several weeks.
Common Causes of an Infected Wisdom Tooth
| Cause | Description | Likelihood |
|---|---|---|
| Impaction | Wisdom teeth that do not fully emerge, trapping food and bacteria beneath the gum | High |
| Poor Oral Hygiene | Inadequate brushing or flossing allows plaque to accumulate and bacteria to thrive | Medium |
| Gum Trauma | Injury or irritation to the surrounding gum tissue that can increase infection risk | Low |
| Pre-existing Dental Conditions | Cavities or gum disease in adjacent teeth can exacerbate infections | Medium |
| Dry Mouth (Xerostomia) | Reduced saliva production can allow bacteria to proliferate more easily | Low |
| Dietary Factors | High sugar intake can contribute to bacterial growth around partially erupted teeth | Medium |
Diagnosing an Infection During Waiting Times
Visual Self-Checks at Home
While waiting for a polyclinic appointment, you can perform a simple self-examination. Use a bright light and mirror to inspect the back molars for redness, swelling, or pus. Gently floss around the affected area to check for bleeding or tenderness. While self-checks cannot replace a professional diagnosis, they can help you monitor infection progression and identify red flags early.
Pain Assessment and Tracking Changes
Tracking your symptoms daily can provide valuable information for your dentist. Note the intensity, location, and timing of pain. This can help differentiate between normal eruption discomfort and a true infection. Pain that intensifies or becomes persistent over several days usually warrants prompt professional evaluation.
When to Use Over-the-Counter Relief Safely
Over-the-counter (OTC) analgesics like ibuprofen or paracetamol can temporarily manage pain and reduce mild inflammation. Always follow the recommended dosages on the packaging, and avoid excessive use. While these medications do not treat the underlying infection, they can provide short-term relief and make the waiting period more tolerable.
Red Flags That Require Urgent Attention
Immediate medical attention is necessary if you notice any of the following symptoms:
- High fever or chills
- Rapidly increasing swelling in the jaw, cheek, or neck
- Difficulty swallowing or breathing
- Severe, unrelenting pain or pus discharge
These signs may indicate a spreading infection that could have serious health implications if left untreated.
Managing Discomfort While Waiting for a Polyclinic Appointment
Pain Relief Options (OTC medication, cold compress)
If you’ve been unsure about how to know if your wisdom tooth is infected, jaw tenderness is often one of the earliest warning signs linked to wisdom tooth infections and increasing tooth inflammation. OTC painkillers such as ibuprofen or paracetamol can alleviate mild to moderate pain. Additionally, topical gels containing benzocaine may numb the affected area temporarily. External cold compresses applied to the cheek near the infected tooth for 10–15 minutes several times a day can help reduce swelling and discomfort. Always avoid applying ice directly to the skin to prevent frostbite.
Oral Hygiene Measures to Reduce Tooth Inflammation
Maintaining oral hygiene is essential even when pain makes brushing uncomfortable. Rinse your mouth with warm saltwater (1 teaspoon of salt in a glass of warm water) 2–3 times daily to reduce bacterial load. Use a soft-bristled toothbrush to gently clean around the infected tooth, avoiding aggressive scrubbing that could worsen inflammation. Antiseptic mouthwashes can also help, but avoid alcohol-based products if your gums are sensitive.
Diet and Eating Adjustments
Soft, non-acidic foods can ease discomfort while ensuring nutrition. Suitable options include mashed potatoes, yoghurt, soups, smoothies, and soft-cooked vegetables. Avoid hard, crunchy, or sticky foods that may irritate the affected area or get trapped around the wisdom tooth.
Avoiding Activities That Worsen the Infection
Activities that increase bacterial exposure or mechanical stress can exacerbate symptoms. Refrain from smoking, chewing gum, using the affected side heavily, or attempting to manually remove trapped food with sharp objects. These actions can increase the risk of spreading the infection or triggering an abscess.
When to Seek Immediate Dental Care
Some symptoms indicate that a wisdom tooth infection may be spreading or worsening, requiring urgent professional intervention. Seek immediate dental care if you experience:
- Rapidly worsening swelling or redness in the jaw or face
- High fever or chills
- Difficulty breathing or swallowing
- Severe pain unresponsive to OTC medication
- Persistent pus discharge
Delaying treatment in such cases can result in serious complications such as cellulitis, systemic infection, or jaw abscesses, which may require hospital-based care.
Prevention Tips for Wisdom Tooth Infections
Maintaining Good Oral Hygiene Around Wisdom Teeth
Brush twice daily, floss carefully around the back molars, and consider using an interdental brush to remove food particles trapped near partially erupted teeth. Rinsing with antiseptic mouthwash can further reduce bacterial buildup and prevent inflammation.
Routine Dental Checkups to Catch Early Tooth Inflammation
Regular dental visits every 6–12 months allow dentists to monitor wisdom teeth before problems develop. X-rays can detect impacted teeth, early decay, or signs of tooth inflammation. Early intervention can prevent infections, reduce pain, and minimise the need for complex procedures.
Lifestyle Habits That Reduce Risk of Infection
A balanced diet, limiting sugary and acidic foods, maintaining adequate hydration, and avoiding smoking all contribute to oral health. Smoking cessation, in particular, reduces gum disease risk and enhances the healing capacity of oral tissues. Additionally, wearing mouthguards during sports and maintaining overall immune health can help prevent infections.
Frequently Asked Questions
1. How can I tell if my wisdom tooth is infected or just sore?
While mild soreness can occur during tooth eruption, infection typically presents with multiple symptoms such as swelling, redness, pus discharge, persistent pain, and bad breath. Observing symptom progression over several days and keeping a record can help distinguish normal discomfort from infection.
2. Can tooth inflammation go away without treatment?
In some cases, mild inflammation may temporarily subside with improved oral hygiene and OTC pain relief. However, bacterial infections rarely resolve completely without professional care. Untreated infections may worsen and result in abscess formation or spread to surrounding tissues.
3. Are wisdom tooth infections dangerous if untreated?
Yes. Untreated infections can extend to adjacent teeth, jawbone, and facial tissues. Severe infections can enter the bloodstream, leading to sepsis, which is life-threatening. Early intervention is crucial to prevent these outcomes.
4. What can I do at home while waiting for a dental appointment?
At home, maintain oral hygiene, rinse with warm saltwater, use OTC painkillers appropriately, apply cold compresses, eat soft foods, and avoid activities that aggravate the area. Monitoring symptoms daily ensures you can seek urgent care if red flags appear.
5. How long does it usually take to recover from a wisdom tooth infection?
Recovery varies based on infection severity and treatment. Mild infections may resolve in 3–5 days post-treatment, while severe cases requiring antibiotics or extraction may take 1–2 weeks or more for full recovery. Following your dentist’s care plan is essential for faster healing.